Umbilical Hernia in Patients with Berardinelliseip Syndrome: Is it Really Hernia
Josivan Gomes de Lima, Natalia Nobrega de Lima, Camila Frade Oliveira, Ruth Ellen Fernandes Castro Dantas, Maria de Fátima Paiva Baracho, Lúcia Helena Coelho Nóbrega, Selma Maria Bezerra Jeronimo
1Departamento de Medicina Clínica, Hospital Universitário Onofre Lopes, UFRN, Natal-RN, Brazil
2Instituto de Medicina Tropical (IMT), Departamento de Bioquímica, UFRN, Natal-RN, Brazil
Received Date: November 12, 2015; Accepted Date: December 10, 2015; Published Date: December 18, 2015
Citation: de Lima JG, de Lima NN, Oliveira CM, et al. Umbilical Hernia in Patients with Berardinelliseip Syndrome: Is it Really Hernia. J Clin Mol Endocrinol. 2015, 1:1. doi: 10.21767/2572-5432.100001
Copyright: © 2015 de Lima JG, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Umbilical hernia is often described in several cases of Berardinelli-Seip congenital lipodystrophy (BSCL). The aim of this article is to identify whether BSCL patients have umbilical herniation or protrusion.
Cases and methods. We clinically evaluated twelve BSCL patients (eight females) through abdominal palpation sensitized by Valsalva maneuver. None of them had a history of surgical treatment for umbilical hernia repair neither complained of symptoms such as pain, abdominal discomfort, nausea, nor vomiting. We did not find any case of umbilical hernia, but all of them had protrusion of the umbilicus. Conclusion. At least in our patients, umbilical hernia is not part of BSCL and patients truly have protrusion of the umbilicus due to the almost complete absence of subcutaneous fat tissue.
Keywords
Hernia; Lipodystrophy; Diabetes
Introduction
Berardinelli-Seip congenital lipodystrophy (BSCL) is an autosomal recessive disease that causes a general decrease in body fat. It was first described in Brazil in 1954 and five years later in Norway [1-3]. There are four types according to the mutations in genes of AGPAT2, seipin, caveolin-1 and cavin-1 (Types 1, 2, 3 and 4, respectively) [4]. These mutations cause defects in triglyceride synthesis, formation of lipid droplets, and differentiation/ development of adipocytes, resulting in hypertriglyceridemia, insulin resistance, diabetes and hepatosplenomegaly [4].
The prevalence of BSCL is about 1 in 10 million, and there are between 300 and 500 cases reported in the literature [4]. However, in our region, due to frequent consanguineous marriage, the prevalence is higher than the rest of the world, reaching 1:128000 [5,6]. Umbilical hernia is often described in several cases [1], but we have followed around 53 patients with BSCL the past 17 years and did not find any. Hernia, by definition, is a circumscribed mass formed by an organ (or a part of an organ) exiting, naturally or accidentally, through an orifice from the cavity that contains it. Instead of this, an umbilical protrusion is characterized by the presence of a palpable mass, but without organs therein. The aim of this article is to identify whether BSCL patients have umbilical herniation or protrusion.
Cases and Methods
We evaluated twelve patients diagnosed with BSCL (eight females) and followed up during the last two years. The median of age was 19.7 ± 10.6 years old (ten adults and two children). Inclusion criteria were BSCL mutation identified and possibility of clinical examination. We clinically evaluated patients through abdominal palpation, sensitized by Valsalva maneuver. Three patients had a mutation in the AGPAT2 (BSCL Type 1), and the other nine patients had a mutation of seipin (BSCL Type 2). Nine patients (75%) were diabetic, and four (33.3%) had arterial hypertension. None of the patients had a history of surgical treatment for umbilical hernia repair neither complained of symptoms such as pain, abdominal discomfort, nausea, nor vomiting.
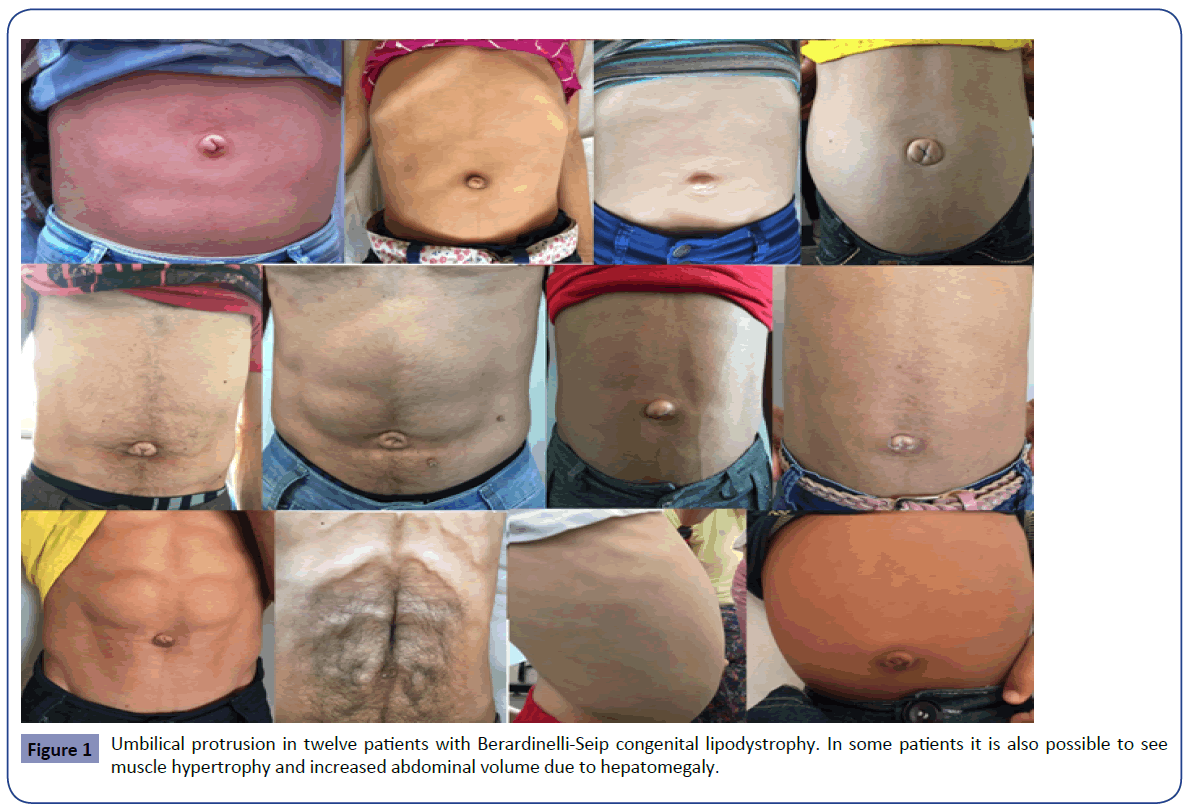
The body mass index was 19.3 ± 4.0 kg/m2 and all patients had an acromegaloid facial appearance, atrophic cheeks (loss of Bichat’s fat ball), muscle hypertrophy, phlebomegaly, and umbilical protrusion (Figure 1). Examination of the abdomen showed an absence of subcutaneous adipose tissue confirmed by Dual-energy X-ray Absorptiometry (DXA) of total body fat of 5.4 ± 0.7%. The majority of patients (66.7%) had acanthosis nigricans and some of them presented abdominal distention due to hepatomegaly (Figure 1). No patient had umbilical hernia on physical examination, but we did not perform abdominal ultrasound.
Fasting glycemia was 108.9 ± 64.8 mg/dl (diabetic patients 120.3 ± 72 mg/dl), glycated hemoglobin 6.5 ± 1.4% (diabetic patients 7.0 ± 1.3%), total cholesterol 161.8 ± 32.8 mg/dl, HDL cholesterol 31.9 ± 4.3 mg/dl and triglycerides 251.4 ± 140.1 mg/dl. Serum insulin was high (27.5 (8.5-115) mUI/ml) and serum leptin was very low (0.94 ± 0.5 ng/ml).
Discussion
We report twelve cases of Berardinelli-Seip syndrome (congenital generalized lipodystrophy) that is a rare autosomal recessive disease. In our region, we have a higher prevalence than that described in the literature [5], and this is probably due to frequent marriages that occur between relatives. Unlike the literature data, we did not find any case of umbilical hernia in our patients [5,6], but all of them had protrusion of the umbilicus due to lack of subcutaneous adipose tissue. Upon inspection at a glance, this protrusion looks like a hernia (Figure 1), then, due to the rarity of the disease, physicians less aware of this syndrome could misdiagnose this protrusion as an umbilical hernia, and this could explain the frequent hernia reports in the literature but not confirmed in our series.
Once we did not perform ultrasound exams to confirm the absence of hernia, it is necessary to think about other possibilities to explain the lack of this diagnosis. First of all, the physical examination could not be sensitive enough to detect the herniation, but in this case, despite the absence of a correct diagnosis, patients should present some symptoms. Pain at the umbilicus (44%), discomfort in the abdomen (20%) and nausea and vomiting (9%) are the most common hernia associated symptoms [7], but no patient had any of these complaints.
If our patients were misdiagnosed and did not have congenital generalized lipodystrophy, this would explain the absence of hernia. However, all patients had clinical features consistent with the diagnosis of BSCL, serum leptin and total body fat very low and showed a confirmed mutation at genetic testing. This rule out the possibility they do not have the syndrome.
We showed only patients with BSCL Types 1 and 2. If umbilical hernia was more frequent in the Types 3 and 4, this could explain the lack of diagnosis in our patients. However, the Types 1 and 2 account for 95% of all reported cases of BSCL [8] and Type 2 (more common in our series) is the most severe type of lipodystrophy. The cases described here are the most common and also represent the most severe types of BSCL [8], and then if umbilical hernia would be part of the syndrome, it should be present.
We showed only twelve patients with BSCL, but we already follow more than fifty cases in our outpatient endocrine clinic in the last seventeen years, and none of these patients required surgical repair of hernia. We did not perform abdominal ultrasound in any patient, but if it had been made and showed any hernia, this would be not very important, once patients did not present symptoms neither had strangulated hernia during follow-up. Since the umbilical hernia prevalence in the general population is 0.5 to 0.8% [9], a BSCL patient could have it, but this would not mean it is part of the syndrome. Umbilical protrusion, instead of umbilical hernia, seems to be an important and frequent finding in patients with congenital generalized lipodystrophy syndrome.
Conclusion
For all these reasons, we believe that, at least in our patients, umbilical hernia is not part of BSCL and patients truly have protrusion of the umbilicus due to the almost complete absence of subcutaneous fat tissue. Hepatomegaly is a common finding in BSCL and may also contribute to this umbilical protrusion, leading to the misdiagnosis of hernia.
References
- Haghighi A, Kavehmanesh Z, Salehzadeh F, Santos-Simarro F, Van Maldergem L, et al. (2015) Congenital generalized lipodystrophy: identification of novel variants and expansion of clinical spectrum. Clin Genet.
- Berardinelli W (1954)An undiagnosed endocrinometabolic syndrome: report of 2 cases. J ClinEndocrinolMetab 14:193-204
- Seip M (1959)Lipodystrophy and gigantism with associated endocrine manifestations. A new diencephalic syndrome?ActaPaediatr 48:555-574
- Patni N, Garg (2015 ) A Congenital generalized lipodystrophies-new insights into metabolic dysfunction. Nat Rev Endocrinol 11:522-534
- Baracho MF, Nunes AB, Hirata MH, Hirata RD, Fajardo CM, et al. (2014) Association between Pro12Ala, Pvull, Avall, Sstl and ADIPOQ single-nucleotide polymorphisms with lipid and glycemic profiles of patients with Berardinelli-Seip syndrome. Ann NutrMetab 65:272-279
- Faria CA, Moraes RS, Sobral-Filho DC, Rego AG, Baracho MF, et al. (2009) Autonomic modulation in patients with congenital generalized lipodystrophy (Berardinelli-Seip syndrome)Europace 11:763-769
- Rodriguez JA, Hinder RA (2004)Surgical management of umbilical hernia. Operative techniques in general surgery 6:156-164
- Boutet E, El Mourabit H, Prot M, Nemani M, Khallouf E, et al. (2009)Seipin deficiency alters fatty acid Delta9 desaturation and lipid droplet formation in Berardinelli-Seip congenital lipodystrophy. Biochimie 91:796-803
- Burcharth J, Pedersen MS, Pommergaard HC, Bisgaard T, Pedersen CB, et al. (2015) J. The prevalence of umbilical and epigastric hernia repair a nationwide epidemiologic study. Hernia 19:815-819.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences