Cardiometabolic Indices Among Ageing Nigerians with Type 2 Diabetes in a Tertiary Health Facility
Abimbola Lawal
Department of Medicine, University College Hospital, Ibadan, Nigeria
Published Date: 2023-04-27DOI10.36648/2572-5432.8.1.87
Williams O Balogun, Martins E Emuze, Abimbola Lawal* and Ejemhen I Ekhaiyeme
Department of Medicine, University College Hospital, Ibadan, Nigeria
- *Corresponding Author:
- Abimbola Lawal
Department of Medicine,
University College Hospital, Ibadan,
Nigeria,
E-mail: debbimlaw@gmail.com
Received date: March 27, 2023, Manuscript No. IPJCME-23-16159; Editor assigned date: March 30, 2023, PreQC No. IPJCME-23-16159 (PQ); Reviewed date: April 13, 2023, QC No. IPJCME-23-16159; Revised date: April 20, 2023, Manuscript No. IPJCME-23-16159 (R); Published date: April 27, 2023, DOI: 10.36648/2572-5432.8.1.87
Citation: Balogun WO, Emuze ME, Lawal A, Ekhaiyeme EI (2023) Cardio Metabolic Indices among Ageing Nigerians with Type 2 Diabetes in a Tertiary Health Facility. J Clin Mol Endocrinol Vol.8 No.1: 87
Abstract
Age related hyperglycemia has been described among elderly people with the main pathophysiologic mechanisms being peripheral insulin resistance, pancreatic β cell secretory defect, reduced islet cell proliferative capacity with aging, adiposity, sarcopenia/sarcopenic obesity, physical inactivity and age-associated reduced muscle mitochondrial function.
The increased risk of microvascular and macrovascular complications, hypoglycemia and higher risk of mortality in the elderly has a significant impact on approach to their disease management.
We evaluated 127 elderly subjects in a retrospective crosssectional study at a foremost Geriatric Center in UCH, Ibadan.
The overall median (range) duration of diabetes was 8 (0.25-40) years. The duration of diabetes increased across the age groups. There were no significant differences between the male and female participants in most parameters including BMI, waist circumference, systolic and diastolic blood pressures glycemic profile and eGFR. The 70 years-79 years age group had higher BMI, waist circumference and blood pressure though with no statistical significant differences.
The LDL cholesterol and triglycerides were significantly different among the age groups, with LDL cholesterol being highest in the >80years group. The women had significantly higher total cholesterol than males: 168.5 ± 42.5 vs 198.0 ± 48.0 respectively. Overall, the systolic blood pressure, LDL cholesterol and all the glycaemic indices indicate suboptimal control.
Across the three age groupings, the glycaemic profile and eGFR progressively decrease from 60 years-69 years to >80 years suggesting declining renal function and higher risk of hypoglycaemia with increasing age.
This study highlights the cardio-metabolic risks among the elderly with diabetes and the need to tailor their treatment accordingly.
Keywords
Diabetes; Hyperglycemia; Obesity
Introduction
Diabetes Mellitus (DM), one of the common chronic diseases that have affected many people worldwide, with impact on all ages has continued to be a condition with great public health concern globally [1]. Different classifications exist for DM, out of which Type 2 Diabetes Mellitus (T2DM) is regarded as the commonest, accounting for over 90% of the persons with DM [1,2]. The world has witnessed a progressive increase in the prevalence of DM and this has been projected to rise further in the coming years both on a global scale and in different parts of the world, including Africa. In addition, the prevalence of diabetes increases with age, with the highest prevalence noted in elderly patients above 65 years old and this is expected to accelerate further over the next 25 years, though currently put at 24% [1].
Diabetes is a leading cause of cardiovascular disease, blindness, kidney failure and lower limb amputation in older adults [1,3]. High proportions of Nigerians living with diabetes have multiple cardiovascular risk factors as well as complications and have sub-optimal glycaemic control [4]. Urban residence and increasing socioeconomic status were identified as risk factors for new onset diabetes among elderly Nigerians [5].
A percentage of elderly people have been termed to have age-associated hyperglycemia which is likely to be a spectrum between normality and T2DM [6]. T2DM is a product of interaction between genetic and environmental factors and main pathophysiologic mechanisms in elderly population and others involve peripheral insulin resistance and pancreatic β cell secretory defect [7-10]. There is also reduced islet cell proliferative capacity with aging [11,12]. Adiposity, sarcopenia/ sarcopenic obesity, physical inactivity, age-associated reduced muscle mitochondrial function have been shown to contribute to insulin resistance in the elderly [2,9].
Inflammatory markers like TNF-α has been strongly correlated with insulin resistance in obese elderly patients with diabetes [7,13]. People with obesity, those who consume diets that are high in saturated fat and low in complex carbohydrates, or who are inactive are more likely to develop diabetes as they age [7]. Variations in glucose metabolism in elderly patients with diabetes mellitus have been reported in some studies, especially when compared to middle-aged patients with diabetes [14-16]. Interestingly, one-half of older persons with diabetes are undiagnosed as classical symptoms of hyperglycemia may not be present in the elderly population probably because the renal threshold for glucose increases with age, impairment of thirst with normal aging making polydipsia unlikely [7,17]. There is increased risk of both microvascular (retinopathy, neuropathy, nephropathy) and macrovascular complications (cardiovascular disease, cerebrovascular disease, peripheral arterial disease) in elderly patients with diabetes compared with controls and this has been correlated with duration of diabetes, HbA1c values and the presence of traditional risk factors such as smoking, hypercholesterolaemia and hypertension [1,7,17]. Thus, it could be mentioned that there appears to be existing differences between demographic and clinical characteristics of older adults with diabetes and those diagnosed in middle age, which may impact on approach to disease management in this group of people. Despite the projected significant increase in the diabetes population of the ageing societies in the coming years and the inevitable public health and economic challenges, not much information is available in sub-Saharan Africa, Nigeria inclusive on the clinical and metabolic characteristics of elderly patients with DM. The aim of this study is to determine the frequencies of abnormal cardio-metabolic indices among Nigerian older adults with type 2 diabetes attending Geriatric Centre, University College Hospital, Ibadan.
Materials and Methods
Study locat on and design
This was a retrospective cross-sectional study that was carried out at the outpatient diabetes clinic of the Chief Tony Anenih Geriatric Centre (CTAGC) at the University College Hospital, (UCH) Ibadan. UCH is the premier teaching hospital which serves the Ibadan environs and the country at large and also a referral centre in southwest geopolitical zone of Nigeria. The CTAGC is the pioneer Geriatric Centre in the West African sub-region established in November 2012. It was purposely built to take care of the health needs of the adults in Geriatric age group (senior citizens aged 60 years and above).
Data collect on procedure
Health records of older adults aged 60 years and above, diagnosed to have diabetes mellitus according to WHO clinical criteria, who were seen at the Diabetes Outpatient Clinic of the CTAGC, UCH, Ibadan within a 2-year period (May 2019-April 2021) were accessed. Relevant data were captured from the clinic diabetes registry. A questionnaire proforma was used to obtain the data with regards to socio-demographic characteristics ((age, gender, etc.), clinical (weight, height, blood pressure, etc.) and laboratory profiles of the patients including fasting lipid profile, FPG and 2-hour PPG, serum creatinine and glycated hemoglobin). All clinical chemistry analytes were done at the central laboratory of the hospital using standard assay procedures on automated Roche machine. The duration of diabetes was also documented. History of hypertension, cardiovascular risk factors and diseases and drug history were obtained.
Ethical approval for the study was obtained from the Joint University of Ibadan/University College Hospital Institutional Ethical Review Board (UI/UCH IRB).
Criteria for sub-optimal cardio-metabolic risk factors were defined as follows:
The Body Mass Index (BMI): Which is the weight in kilograms divided by the square of the height in metres (kg/m2) was calculated and classified as underweight, normal weight, overweight, obese and extremely obese based on BMI values <18.5, 18.5-24.9, 25.0-29.9, 30-39.9 and ≥ 40 kg/m2 respectively
Blood Pressure: A resting systolic blood pressure of ≥ 130 mmHg and/or a diastolic blood pressure of ≥ 85 mmHg.
Lipid Profile: Triglyceride >150 mg/dl (1.7 mmol/L); Total cholesterol >200 mg/dl (5.2 mmol/L); LDL-cholesterol >135 mg/dl (>3.5 mmol/L); HDL-cholesterol <40 mg/dl in men and <50 mg/dl in women.
Fasting plasma glucose: >120 mg/dl.
Two-hour postprandial glucose: >160 mg/dl.
Haemoglobin A1c: >7%.
Data analysis was conducted using the statistical software for the social sciences version 25.0.
Statistical analysis
Data analysis was conducted using the statistical software for the social sciences version 25.0.
Descriptive statistics were summarized using frequency tables. Bivariate analyses (using Chi-square tests) were used to determine the association between respondents’ characteristics and glycemic control (good or poor glycemic control). Student’s t- and/or analysis of variance tests as applicable were used to compare the means of glycemic control and respondents’ clinical characteristics, including the mean duration of diabetes, body mass index, waist circumference, systolic blood pressure, diastolic blood pressure, total cholesterol, triglycerides, low density lipoprotein, high density lipoprotein and glomerular filtration rate. P-values <0.05 were regarded as statistically significant.
Results
Overall, 95 (73.1%) of the participants were females; 41 (78.8%) of those aged 60 years-69 years were females, compared to 37 (66.1%) aged 70 yeaars-79 years and 14 (73.7%) aged ≥ 80 years (Table 1). The overall median (range) duration of diabetes was 8 (0.25-40) years. The duration of diabetes increased across the age groups. There were no significant differences between the male and female participants in most parameters including BMI, waist circumference, systolic and diastolic blood pressures glycemic profile and eGFR. However, compared to the men, the women had significantly higher total cholesterol: 168.5 ± 42.5 and 198.0 ± 48.0 for males and females respectively.
| Characteristic | Males | Females | P |
|---|---|---|---|
| N=35 (27.6%) | N=92 (72.4%) | ||
| Age (years): 60-69 | 11 (21.2) | 41 (78.8) | |
| 70-79 | 19 (34.5) | 37 (66.1) | 0.3 |
| ≥ 80 | 5 (26.3) | 14 (73.7) | |
| Diabetes duration (years) | 11.5 (9.2) | 10.3 (9.3) | 0.56 |
| Family history of DM | 10 (20.4) | 39 (79.6) | 0.11 |
| BMI (kg/m2) | 27.4 (4.8) | 28.3 (4.5) | 0.39 |
| Waist circumference (cm) | 99.7 (11.6) | 99.5 (10.7) | 0.95 |
| Systolic blood pressure (mmHg) | 135.9 (18.8) | 140.1 (23.4) | 0.34 |
| Diastolic blood pressure (mmHg) | 77.7 (10.1) | 79.7 (12.6) | 0.42 |
| Fasting blood glucose (mg/dl) | 160.3 (62.1) | 180.3 (80.6) | 0.22 |
| 2-hour postprandial (mg/dl) | 256.7 (99.4) | 251.7 (111.0) | 0.42 |
| Hemoglobin A1c (%) | 10.0 (3.2) | 9.5 (2.5) | 0.34 |
| Total cholesterol (mg/dl) | 168.5 (42.5) | 198.0 (48.0) | 0.01* |
| Triglycerides (mg/dl) | 117.6 (70.6) | 132.2 (68.1) | 0.38 |
| LDL cholesterol (mg/dl) | 102.8 (35.7) | 119.9 (41.4) | 0.07 |
| HDL cholesterol (mg/dl) | 47.4 (15.5) | 53.8 (18.0) | 0.12 |
| eGFR (ml/min/1.73m2) | 76.1 (25.9) | 76.9 (25.8) | 0.89 |
Table 1: Units of variables.
Table 2 shows the distribution of renal and cardio-metabolic risk factors among the three groups of participants. Overall, the systolic blood pressure, LDL cholesterol and all the glycaemic indices indicate suboptimal control. Generally, the 70 years-79 years age group had higher BMI, waist circumference and blood pressure compared to the other two groups of 60 years-69 years and ≥ 80 years, although with no statistically significant differences.
| Variable | All N= 130 N (%) |
60-69 years n=55 n (%) |
70-79 years n=56 n (%) |
≥ 80 years n=19 n (%) |
|
|---|---|---|---|---|---|
| BMI (kg/m2) | 28.1 ± 4.5 | 28.5 ± 4.1 | 28.0 ± 5.1 | 27.1 ± 4.0 | 0.83 |
| Waist circumference | 99.6 (10.9) | 99.6 (9.8) | 100.3 (12.0) | 96.3 (10.7) | 0.39 |
| Systolic BP (mmHg) | 138.8 ± 21.9 | 136.8 ± 20.7 | 140.8 ± 21.0 | 138.7 ± 27.7 | 0.38 |
| Diastolic BP (mmHg) | 79.1 ± 11.8 | 78.5 ± 11.6 | 80.6 ± 11.1 | 76.3 ± 13.9 | 0.34 |
| Glycemic profile | |||||
| HbA1c (%) | 9.6 ± 2.7 | 10.0 ± 2.6 | 9.6 ± 2.6 | 8.5 ± 3.0 | 0.95 |
| FBG (mg/dl) | 176.1 ± 75.6 | 193.8 ± 86.1 | 166.7 ± 66.5 | 144.8 ± 55.0 | 0.16 |
| Postprandial glucose (mg/dl) | 255.5 ± 105.7 | 275.6 ± 103.4 | 238.1 ± 100.1 | 239.7 ± 120.7 | 0.78 |
| Lipid profile | |||||
| Total Cholesterol (mg/dl) | 191.3 ± 48.3 | 196.0 ± 50.0 | 182.7 ± 50.3 | 203.4 ± 27.9 | 0.12 |
| Triglycerides (mg/dl) | 128.3 ± 68.7 | 135.0 ± 65.4 | 133.2 ± 81.5 | 94.4 ± 20.5 | 0.04* |
| LDL (mg/dl) | 115.5 ± 40.1 | 122.2 ± 45.9 | 104.2 ± 31.4 | 128.3 ± 34.2 | 0.01* |
| HDL | 52.1 (17.5) | 49.9 (17.5) | 52.1 (17.3) | 60.6 (17.0) | 0.94 |
| eGFR | 76.7 (25.7) | 80.1 (26.0) | 75.3 (25.7) | 70.7 (25.2) | 0.92 |
| Note: BP: Blood Pressure; LDL: Low Density Lipoprotein; HDL: High Density Lipoprotein; eGFR: estimated Glomerular Filtration Rate; BMI: Body Mass Index; FG: Fasting Blood Glucos; HbA1c: Haemoglobin A1c. | |||||
Table 2: Distribution of cardio metabolic risk factors among the age categories.
Across the three age groupings, the glycaemic profile (HbA1c, fasting and 2-hour postprandial glucose) and eGFR progressively decrease from 60 years-69 years to >80 years. The LDL cholesterol and triglycerides were significantly different among the age groups, with LDL cholesterol being highest in the ≥ 80 years group while triglyceride was highest among those 60 years-69 years.
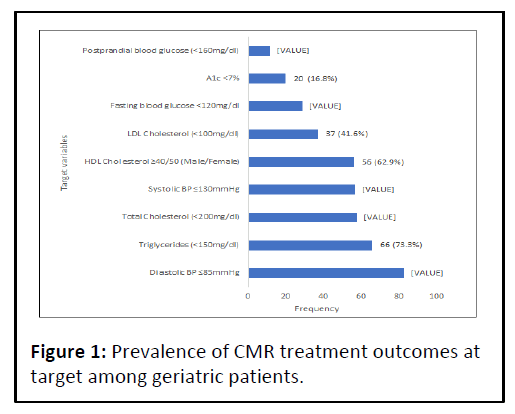
In Figure 1, the frequencies of at target CMR factors among the participants are displayed. Haemoglobin A1c and triglyceride had the least and highest percentages {20 (16.8%) and 66 (73.3%)} respectively of these geriatric patients at treatment targets of the 119 (95.0%) patients with documented weights, 21 (17.6%) had normal BMI (<25 kg/m2), while 98 (82.4%) had excess weight (BMI>25 kg/m2).
Discussion
Diabetes mellitus is the sixth most common cause of death among adults who are elderly and cardiovascular diseases constitute a major cause of mortality [7,18]. Age-related alterations in carbohydrate metabolism, including changes in glucose-induced insulin release and resistance to insulinmediated glucose disposal, in association with genetics account for the increase in diabetes incidence with the aging process [7]. Hyperglycemia, dyslipidemia, obesity, insulin resistance, inflammation, hypertension, autonomic dysfunction and diminished vascular responsiveness have been identified as contributory factors to CVD risk in diabetes [18]. The aim of this study is to determine the frequencies of abnormal cardiometabolic indices among older adults with type 2 diabetes attending a Geriatric Centre in Nigeria.
More of the participants in our study were females (73.1%) similar to a study by Enang, et al., in Lagos, Nigeria on elderly patients with diabetes [19]. In contrast, Jain, et al., in India reported equal "numbers" of male and females with diabetes [20].
This may be due to an improved health seeking behavior among the women, the reported slightly higher prevalence of DM in African female older adults than the male counterparts and/or the fact that some of the women were widows who might have lost their spouses to cardiovascular diseases and would want to prevent further occurrence via improved health care attendance [1,20,21].
The median duration of DM was 8 years in this study and it is important to note that the longer the duration of DM, the higher likelihood of patients manifesting with complications, especially in the setting of advancing age [22]. Furthermore, Hateren, et al., reported that among elderly diabetes patients with a disease duration of 8 years and longer, higher lipids were predictive of increased cardiovascular mortality [23].
The study showed no significant difference between male and female participants as regards BMI, waist circumference, glycaemic profile and blood pressure. This is similar to a study by Kumar, et al., in India about incidence of metabolic syndrome and its characteristics among patients with DM where similar BMI and blood pressure were recorded for both males and females [24]. However, Alamgir, et al., in Pakistan had contrary results where female patients with T2DM were found to be overweight, have higher blood pressure and uncontrolled hyperglycemia when compared to their male counterparts [25]. This may be due to the fact that much older patients were not included in their study (none of the participants was older than 65 years).
Generally, our study showed a suboptimal glycaemic control (FBG, postprandial blood glucose and HbA1c) among the participants with about 16.8% reaching the HbA1c target, comparable to report by Zhu, et al., in China and Alamgir, et al., in Pakistan [25,26]. A prominent feature of type 2 diabetes in older adults is postprandial hyperglycemia, [2,10,27] and some prospective epidemiologic studies have demonstrated a strong correlation between HbA1c values and the risk of complications in elderly population [7,17]. It has been proposed that elderly patients with shorter duration of type 2 diabetes and without established atherosclerosis might have cardiovascular benefit from intensive glycemic control, but potential risks of intensive glycaemic control may outweigh its benefits in other patients with a very long duration of diabetes, known history of severe hypoglycemia, major comorbid illness, advanced atherosclerosis and advanced age/frailty [2,28].
The glycaemic control across the age groups in our study maintained a downward trend (though suboptimal), similar to a retrospective study of elderly T2DM persons by Huang, et al., in the North California Diabetes registry, where older patients had lower HbA1c values [29]. An explanation could be the likelihood that older persons had shorter duration of diabetes or may also be on insulin. Generally, this finding looks atypical considering the expected worsening of glycaemic control with diabetes duration or advanced age. It is possible that other factors that could affect metabolic control like medication adherence, other comorbities like chronic kidney disease and lifestyle changes differ across the age groups as well [26].
A decline in eGFR across the age groups was also observed in our study, indicative of declining renal function (manifesting as Chronic Kidney Disease-CKD) with prolonged duration of DM and advanced age, similar to findings from other studies [7,22,29,30]. In the Northern California Kaiser Permanente Diabetes Registry of older people with T2DM, Huang, et al., reported that CKD stage 3 (eGFR 30–59 ml min-1 [1.73 m]-2) was found in 32% and CKD stage 4 (eGFR 15–30 ml min−1 [1.73 m]−2) in 2.6% of participants. This underscores the importance of monitoring for detection of CKD when it sets in and the need for follow up, which may be instructive as regards selection of the appropriate glucose-lowering agent, prevention of hypoglycemia and dose adaptation when progression of kidney impairment occurs. Apart from glycaemic control and advanced age, exposure to higher blood pressures also serves as a risk factor for CKD, especially in this study where the systolic BP was largely suboptimal [31].
Compared to the males in our study, the females have significantly higher level of total cholesterol and this is in agreement with report by Alamgir, et al., in Pakistan, Loh, et al., in Singapore, Habib, et al., in Saudi Arabia and Ogbera, et al., in Nigeria [25,31-33]. Dietary and lifestyle factors like a sedentary living, reduced activity, hormonal factors in female subjects may be contributory to the findings [25,31,32]. It has been discovered that a steep rise of total cholesterol occurs around menopause in women, and is majorly determined by the increase in LDL-cholesterol concentration [31,34]. This may have an implication for worsened cardiovascular events among the women.
The 70 years-79 years age group had higher anthropometry and blood pressure compared to the other groups, which is almost similar to findings by Hateren, et al., [23]. It is likely that patients in this group have less frailty and sarcopenia, which may be challenges with much older adults who are at least 80 years old [2,30].
There was significant difference among the age groups concerning low density lipoprotein and triglyceride, with the LDL being highest in the older adults at least 80 years old while the TG was highest in the 60 years-69 years age group. This is in line with another study by Zafar, et al., where elevated LDL was reported with increasing age of subjects with DM up to the older age group. Considering that there are more females in this study with significantly higher total cholesterol level, the finding about the LDL may not be surprising since total cholesterol is mostly determined by the level of LDL [31,34,35]. The highest level of triglyceride was recorded in the 60 years-69 years group and not the oldest group probably because of likely reduced appetite/meal intake, weight loss with advancing age, as well as variation in body composition [2,30,36]. Alamgir, et al., had also reported increased TG level with age and highest in 55-64 age group [25]. In addition, 73.3% of participants in our study attained the triglyceride target (highest cardio-metabolic risk factor target reached), higher than 54% reported by Mohamed, et al., in Malaysia, despite the younger patients in their study than this study [37].
As regards BMI, about three-quarters of the participants were overweight and obese, similar to report by Bays, et al., [38]. This is however, higher than what was reported from another Nigerian study by Enang, et al., where 68% of elderly patients with T2DM have at least BMI 25 kg/m2 but it is notable that the sample size was smaller than this present study [19]. Dietary and lifestyle factors with effect of urbanization over the years might have resulted in the increasing BMI [1,5,7,26].
Conclusion
This study has revealed varied outcomes in terms of cardiometabolic indices. While dyslipidaemia remains a major risk factor for cardiovascular disease it appears the heterogenous findings in elderly patients with DM suggest that apart from lipid profile, other factors like duration of DM have a role to play in predicting cardiovascular morbidity or mortality. According to Hateren, et al., in their study, dyslipidaemia correlates with cardiovascular mortality for younger elderly patients but for older adults, duration of DM looks important as higher lipid levels were related to increased mortality with duration of DM at least 8 years.
References
- International Diabetes Federation (2021) IDF Diabetes Atlas. (10th ed), International Diabetes Federation, Brussels, Belgium.
- Kirkman MS, Briscoe VJ, Clark N, Florez H, Haas LB, et al. (2012) Diabetes in older adults. Diabetes care 35: 2650-2664.
[Crossref], [Google Scholar]
- https://diabetesatlas.org/
- Chinenye S, Young E (2011) State of diabetes care in Nigeria: A review. Nigerian Health Journal 11:101-106.
- Balogun WO, Gureje O (2013) Self-reported incident type 2 diabetes in the Ibadan study of ageing: Relationship with urban residence and socioeconomic status. Gerontology 59:3-7.
[Crossref], [Google Scholar], [Indexed]
- Lipson LG (1986) Diabetes in the elderly: Diagnosis, pathogenesis and therapy. Am J Med 80:10-21.
[Crossref], [Google Scholar], [Indexed]
- Meneilly GS, Tessier D (2001) Diabetes in elderly adults. J Gerontol A Biol Sci Med Sci 56: M5-M13.
[Crossref], [Google Scholar]
- Defronzo RA (2009) Banting lecture. From the triumvirate to the ominous octet: A new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 58: 773-795.
[Crossref], [Google Scholar], [Indexed]
- Yokono K (2013) Concept and clinical characteristics of diabetes mellitus in the elderly. Nihon rinsho 71: 1893-1898.
- Chang AM, Halter JB (2003) Aging and insulin secretion. Am J Physiol Endocrinol Metab 284: E7-E12.
[Crossref], [Google Scholar], [Indexed]
- Maedler K, Schumann DM, Schulthess F, Oberholzer J, Bosco D, et al. (2006) Aging correlates with decreased β-cell proliferative capacity and enhanced sensitivity to apoptosis: A potential role for Fas and pancreatic duodenal homeobox-1. Diabetes 55: 2455-2462.
[Crossref], [Google Scholar]
- Rankin MM, Kushner JA (2009) Adaptive β-cell proliferation is severely restricted with advanced age. Diabetes 58: 1365-1372.
[Crossref], [Google Scholar], [Indexed]
- Nilsson J, Jovinge S, Niemann A, Reneland R, Lithell H (1998) Relation between plasma tumor necrosis factor-α and insulin sensitivity in elderly men with non-insulin-dependent diabetes mellitus. Arterioscler Thromb Vasc Biol 18: 1199-1202.
[Crossref], [Google Scholar], [Indexed]
- Meneilly GS, Elliott T, Tessier D, Hards L, Tildesley H (1996) NIDDM in the elderly. Diabetes care 19: 1320-1325.
[Crossref], [Google Scholar], [Indexed]
- Arner P, Pollare T, Lithell H (1991) Different aetiologies of type 2 (non-insulin-dependent) diabetes mellitus in obese and non-obese subjects. Diabetologia 34: 483-487.
[Crossref], [Google Scholar], [Indexed]
- Meneilly GS, Elliott T (1999) Metabolic alterations in middle-aged and elderly obese patients with type 2 diabetes. Diabetes care 22: 112-118.
[Crossref], [Google Scholar], [Indexed]
- Meneilly GS, Tessier D (2000) Diabetes in the elderly. Morley JE, van den Berg L, eds. Contemporary Endocrinology, Endocrinology of Aging. Humana Press, Totowa, NJ: 181-203
- Halter JB, Musi N, Crandall JP, Goldberg A, Harkless L, et al. (2014) Diabetes and cardiovascular disease in older adults: Current status and future directions. Diabetes 63: 2578-2589.
[Crossref], [Google Scholar], [Indexed]
- Enang OE, Olamoyegun MY, Akinlade AT, Kushimo WA, Odusi TA, et al. (2009) Anthropometric indices of the elderly attending a diabetes clinic in Lagos. Endocrine and Metabolism Society of Nigeria: 1-2.
- Jain A, Paranjape S (2013) Prevalence of type 2 diabetes mellitus in elderly in a primary care facility: An ideal facility. Indian J Endocrinol Metab 17: S318-S322.
[Crossref], [Google Scholar], [Indexed]
- Gatimu SM, Milimo BW, Sebastian MS (2016) Prevalence and determinants of diabetes among older adults in Ghana. BMC Public Health 16: 1174.
[Crossref], [Google Scholar], [Indexed]
- Huang ES, Liu JY, John PM, Moffet HH, Karter AJ, et al. (2014) Rates of complications and mortality in older patients with diabetes mellitus: The diabetes and aging study. JAMA Intern Med 174: 251-258.
[Crossref], [Google Scholar], [Indexed]
- van Hateren KJ, Landman GW, Kleefstra N, Logtenberg SJ, Groenier KH, et al. (2009) The lipid profile and mortality risk in elderly type 2 diabetic patients: A ten-year follow-up study. PLoS One 4: e8464.
[Crossref], [Google Scholar], [Indexed]
- Kumar SV, Nagesh A, Leena M, Shravani G (2013) Incidence of metabolic syndrome and its characteristics of patients attending diabetic out patients clinic. J Nat Sc Biol Med 4: 57-62.
[Crossref], [Google Scholar], [Indexed]
- Alamgir MA, Javid RA, Hameed A, Mustafa I (2015) Gender difference in components of metabolic syndrome among patients of type 2 diabetes. Pak J Med Sci 31: 886-890.
[Crossref], [Google Scholar], [Indexed]
- Zhu HT, Yu M, Hu H, He QF, Pan J, et al. (2019) Factors associated with glycemic control in community-dwelling elderly individuals with type 2 diabetes mellitus in Zhejiang, China: A cross-sectional study. BMC Endocr Disord 19: 57.
[Crossref], [Google Scholar], [Indexed]
- Szoke E, Shrayyef MZ, Messing S, Woerle HJ, Meyer C, et al. (2008) Effect of aging on glucose homeostasis: Accelerated deterioration of β-cell function in individuals with impaired glucose tolerance. Diabetes Care 31: 539-543.
[Crossref], [Google Scholar], [Indexed]
- Skyler JS, Bergenstal R, Bonow RO, Buse J, Deedwania P, et al. (2009) Intensive glycemic control and the prevention of cardiovascular events: Implications of the ACCORD, ADVANCE, and VA Diabetes Trials: A position statement of the American Diabetes Association and a scientific statement of the American College of Cardiology Foundation and the American Heart Association. J Am Coll Cardiol 32: 187-192.
[Crossref], [Google Scholar], [Indexed]
- Huang ES, Liu JY, Moffet HH, John PM, Karter AJ (2011) Glycemic control, complications, and death in older diabetic patients: The diabetes and aging study. Diabetes Care 34: 1329-1336.
[Crossref], [Google Scholar], [Indexed]
- Schernthaner G, Schernthaner-Reiter MH (2018) Diabetes in the older patient: Heterogeneity requires individualisation of therapeutic strategies. Diabetologia 61:1503–1516.
[Crossref], [Google Scholar], [Indexed]
- Loh TP, Ma S, Heng D, Khoo CM (2016) Age-related changes in the Cardio-metabolic profiles in Singapore resident adult population: Findings from the National Health Survey. PloS one 11: e0162102.
[Crossref], [Google Scholar], [Indexed]
- Habib SS (2013) Gender difference in lipids and glycemic control in patients with type 2 diabetes. Rawal Med J 38: 22-25.
- Ogbera AO (2010) Prevalence and gender distribution of the metabolic syndrome. Diabetol Metab Syndr 2: 1.
[Crossref], [Google Scholar], [Indexed]
- Akahoshi M, Soda M, Nakashima E, Shimaoka K, Seto S, et al. (1996) Effects of menopause on trends of serum cholesterol, blood pressure and body mass index. Circulation 94: 61-66.
[Crossref], [Google Scholar], [Indexed]
- Zafar ME, Rahman F, Prasad KR, Nehal M (2016) Diabetes accelerates age-related lipid profile disturbances in cardiovascular complications. International Journal of Clinical Biochemistry and Research 3: 154-158.
- Saraç F, Savaş S, Gökdemir B, Akçiçek F (2019) Lipid profile in the elderly and middle-aged patients with type 2 diabetes mellitus in relation with gender. Turk J Endocrinol Metab 23: 222-228.
[Crossref], [Google Scholar]
- Mohamed E, Mohamed M, Rashid FA (2004) Dyslipidaemic pattern of patients with type 2 diabetes mellitus. Malays J Med Sci 11: 44-51.
[Google Scholar], [Indexed]
- Bays HE, Chapman RH, Grandy S (2007) The relationship of body mass index to diabetes mellitus, hypertension and dyslipidaemia: Comparison of data from two national surveys. Int J Clin Pract 61: 737-747.
[Crossref], [Google Scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences