A Descriptive Study on Children with Congenital Adrenal Hyperplasia Attending Assiut University Children Hospital
Ahmed Mohammad Bakhit*, Hanaa Abd el-lateef Mohammad and Kotb Abbas Metwalley
DOI10.21767/2572-5432.100044
Ahmed Mohammad Bakhit*, Hanaa Abd el-lateef Mohammad and Kotb Abbas Metwalley
Pediatrics Department, Faculty of Medicine, Assiut University, Egypt
- *Corresponding Author:
- Ahmed Mohammad Bakhit
Pediatrics Department, Faculty of Medicine
Assiut University, Egypt
Tel: +201000601280
Email: ahmedbakhit92322@yahoo.com
Received date: August 30, 2017; Accepted date: November 01, 2017; Published date: November 08, 2017
Citation: Bakhit AM, Mohammad HA, Metwalley KA (2017) A Descriptive study on Children with Congenital Adrenal Hyperplasia Attending Assiut University Children Hospital. J Clin Mol Endocrinol 2:2. doi: 10.21767/2572-5432.10044
Copyright: © 2017 Bakhit AM. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Congenital adrenal hyperplasia is a group of autosomal recessive disorders that result from the deficiency of one of several enzymes involved in the steroidogenic pathway for cortisol biosynthesis. The most common cause of CAH, accounting for 90% of cases, is 21- hydroxylase deficiency resulting from mutations or deletions in the CYP21A gene [1]. Less common causes of CAH are deficiencies in the enzymes 11β-hydroxylase, 3β- hydroxysteroid dehydrogenase, 17α-hydroxylase, steroidogenic acute regulatory protein, cholesterol sidechain cleavage enzyme and P450-oxidoreductase [2]. The symptoms of disease vary depending on the nature and severity of the enzyme deficiency as well as the sex of the individual. Approximately 75% of infants with classical CAH have the severe salt-wasting form of the disease with shock, dehydration, hyponatremia, and hyperkalemia leading to death [3]. Affected females have varying degrees of virilization of the external genitalia. The remaining 25% have the simple virilizing form of disease which is less severe. Non-classical CAH is generally late onset with symptoms such as hirsutism, infertility, acne and alopecia arising from androgen excess [4]. Untreated babies with classic CAH could experience a life threatening adrenal crisis. However, treatment in the form of replacement hormone therapy (hydrocortisone or dexamethasone to replace cortisol and fludrocortisone to replace aldosterone) corrects the hormone deficiencies [3]. Life-long medication is required to prevent the return of symptoms in individuals with classic CAH. In addition, newborns with ambiguous genitalia in CAH should undergo an appropriate work-up by a medical team consisting of a pediatric endocrinologist, urologist, surgeon, geneticist, and psychologist who should assist parents in making fully informed decisions regarding gender assignment and treatment options such as genital reconstructive surgery [5].
Patients and methods: A descriptive study included children from 1 day to 18 years of age with congenital adrenal hyperplasia attending Assiut University Children Hospital over one year in the period from the 1st of June, 2016 to the 30th of May, 2017. Full thorough history and clinical examination were done to all cases: name, age, sex, residence, consanguinity, history of similar cases in the family, history of previous death due to neglected similar disease, methods of presentation as poor weight gain, poor feeding, persistent vomiting, dehydration and/or shock, convulsions, weight, height, blood pressure, signs of ambiguous genitalia, signs of dehydration, hyperpigmentation and signs of precocious puberty. All cases had been subjected to the following investigations: blood sugar, Na+, K+, blood gases, kidney function tests, karyotyping, hormonal analysis(17 OH progesterone, cortisol a.m and p.m testosterone, ACTH), pelvi-abdominal ultrasonography and magnetic resonanse imaging of the abdomen and pelvis.
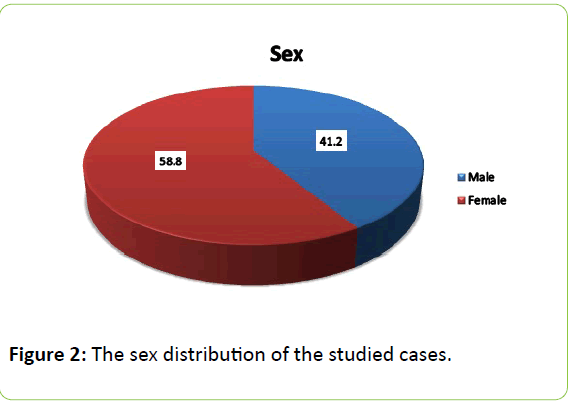
Results: 34 cases of congenital adrenal hyperplasia were included, of whom 8 cases were newly diagnosed on admission while 26 cases were previously diagnosed and came for follow up, 41.2% were males, 58.8% were females.
Congenital adrenal hyperplasia; 17(OH) progesterone; Ambiguous genitalia; Precocious puberty; Salt wasting CAH; Simple virilizing CAH; Non-classic CAH; Adrenal crisis.
Abbreviations
CAH: Congenital Adrenal Hyperplasia; RTA: Renal Tubular Acidosis
Introduction
Congenital adrenal hyperplasia is a group of autosomal recessive disorders that result from the deficiency of one of several enzymes involved in the steroidogenic pathway for cortisol biosynthesis. The most common cause of CAH, accounting for 90% of cases, is 21-hydroxylase deficiency resulting from mutations or deletions in the CYP21A gene [1]. Less common causes of CAH are deficiencies in the enzymes 11β-hydroxylase, 3β-hydroxysteroid dehydrogenase, 17α- hydroxylase, steroidogenic acute regulatory protein, cholesterol side-chain cleavage enzyme and P450-oxidoreductase [2]. The symptoms of disease vary depending on the nature and severity of the enzyme deficiency as well as the sex of the individual [6-9]. Approximately 75% of infants with classical CAH have the severe salt-wasting form of the disease with shock, dehydration, hyponatremia, and hyperkalemia leading to death [3]. Affected females have varying degrees of virilization of the external genitalia. The remaining 25% have the simple virilizing form of disease which is less severe. Non-classical CAH is generally late onset with symptoms such as hirsutism, infertility, acne and alopecia arising from androgen excess [4]. Untreated babies with classic CAH could experience a life threatening adrenal crisis. However, treatment in the form of replacement hormone therapy (hydrocortisone or dexamethasone to replace cortisol and fludrocortisone to replace aldosterone) corrects the hormone deficiencies [3]. Life-long medication is required to prevent the return of symptoms in individuals with classic CAH. In addition, newborns with ambiguous genitalia in CAH should undergo an appropriate work-up by a medical team consisting of a pediatric endocrinologist, urologist, surgeon, geneticist, and psychologist who should assist parents in making fully informed decisions regarding gender assignment and treatment options such as genital reconstructive surgery [5].
Aim
To assess the clinical presentation of children with congenital adrenal hyperplasia attending Assiut University children Hospital. Subjects: Children from 1 day to 18 years of age with congenital adrenal hyperplasia attending Assiut University Children Hospital (From first of June 2016 to end of May 2017).
Inclusion criteria
• In-patients (emergency as salt losing crisis)
• Out-patients (non-emergency as simple virilizing type)
• New cases of CAH
• Previously diagnosed or previously hospitalized cases of CAH
Exclusion criteria
• Other causes of ambiguous genitalia
• Other causes of adrenal insufficiency
• Other causes of failure to thrive
• Other causes of salt losing as RTA
Tools of Study
Full thorough history and clinical examination were done to all cases: name, age, sex, residence, consanguinity, history of similar cases in the family, history of previous death due to neglected similar disease, methods of presentation as poor weight gain, poor feeding, persistent vomiting, dehydration and/or shock, convulsions, weight, height, blood pressure, signs of ambiguous genitalia, signs of dehydration, hyperpigmentation and signs of precocious puberty. All cases had been subjected to the following investigations: blood sugar, Na+, K+, blood gases, kidney function tests, karyotyping, hormonal analysis (17 OH progesterone, cortisol a.m and p.m testosterone, ACTH), pelviabdominal ultrasonography and magnetic resonance imaging of the abdomen and pelvis.
Results
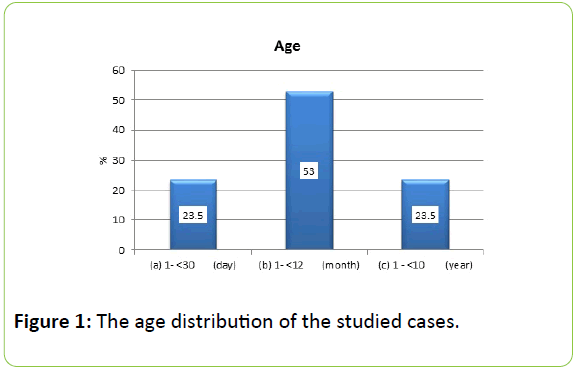
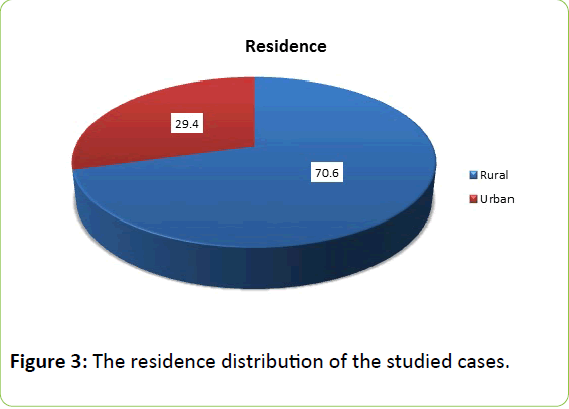
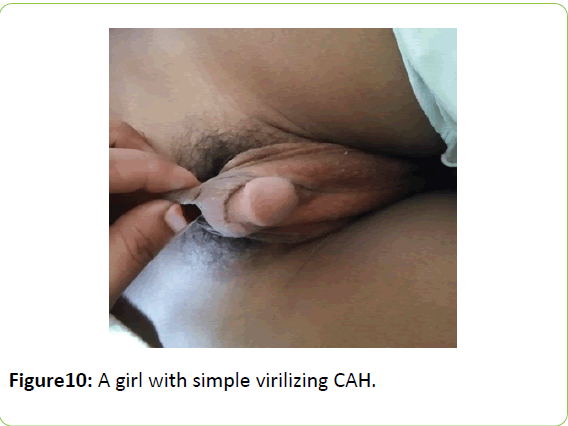
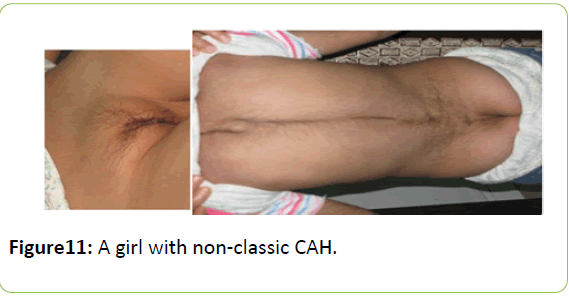
The study was conducted on children from 1 day to 18 years of age with congenital adrenal hyperplasia attending Assiut University Children Hospital over one year in the period from the 1st of June, 2016 to the 30th of May, 2017. The study included 34 cases as shown in Figures 1-11.
A-Demographic data
Discussion
Our study was done on children from 1 day to 18 years of age with congenital adrenal hyperplasia attending Assiut University Children Hospital over one year in the period from the 1st of June, 2016 to the 30th of May, 2017.
During the study period, 34 cases of congenital adrenal hyperplasia were included, of whom 8 cases were newly diagnosed on admission while 26 cases were previously diagnosed and came for follow up, 41.2% were males, 58.8% were females. The female to male ratio was 1.4:1 in our study. Our results are in agreement with other retrospective studies [10] in South East Asia which have reported skewed male: female ratios, with female preponderance; rationale given was that the clinical manifestation was more obvious in females, hence the earlier consult [11] also reported that the female-tomale ratio was 1.25:1 in a retrospective, population-based cohort study done on all known patients with CAH in Sweden between 1910 and 2011 [11].
According to the age at diagnosis in this study, the majority of cases were in the age range 1-12 months by 53% followed by the age range 1-30 days and the age range 1-10 years 23.5% each respectively with mean age at diagnosis 15.15 months. Our results are in agreement with a clinical descriptive study [12] done to determine the sociodemographic, laboratory and clinical characteristics of patients with CAH referred to hospital Putrajaya, a tertiary endocrine center in Malaysia. This study found that median age of patients was 4.1 years with an interquartile range (IQR) of 6, ranging from 1 to 16 years whilst median age at diagnosis of CAH was two years (IQR=1), ranging from 0 to 4 years.
Positive consanguinity was found in 26 cases (76.5%). 1999 [6] reported that the expected high incidence of CAH in Egypt as most Arab countries is due to increased rates of consanguineous marriage (33%) and even higher in Upper Egypt (up to 60%). This is in agreement with [13] who partially attributed this unexpected high incidence of a potentially salt-wasting disorder in a tropical country to consanguinity which is frequent in the Malay- and Indian-, but not in the Chinese community and also hypothesized selective advantage of the heterozygote state as a possible cause.
Positive history of similar cases in the family was found in 13 cases (38.2%). Our results are in agreement with the previously mentioned clinical descriptive study [12] done on fifty-one patients with a diagnosis of CAH during their 3 - 4 monthly clinic visits to the pediatric endocrine clinics at hospital Putrajaya, Malaysia over a period of 12 months. This study found that 31 families had only one child affected with CAH (17 Malays, 8 Chinese, 4 Indians, 2 others), 17 families had two children with CAH (10 Malays & 7 Chinese) while three Malay families had three children with CAH.
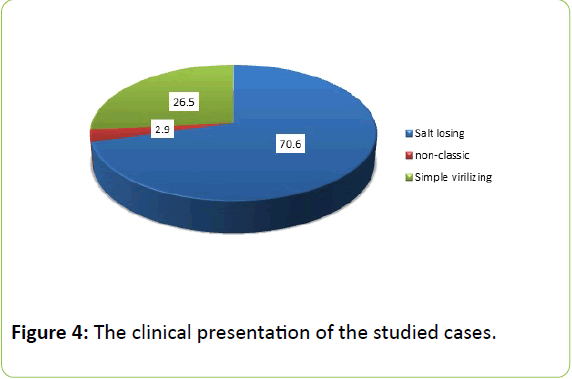
Salt losing type of CAH was found in 24 cases (70.6%) and simple virilizing type was found in 9 cases (26.5%) with ratio of 2.7:1. This is in agreement with [7] who reported that classic salt wasting phenotype accounts for 75% of all cases of classic CAH. Studies from developed countries [14-16] showed the same ratio to be almost 2:1, that is, the SW type of the disease was almost twice more common than the SV type of the disease. However, other studies from India and Singapore [17,18] reported that the ratio of SW type to SV type of disease was 1:1.6 and 1:1.8, respectively. This suggested that a substantial proportion of patients with SW type of disease, particularly males, probably died before diagnosis [19].
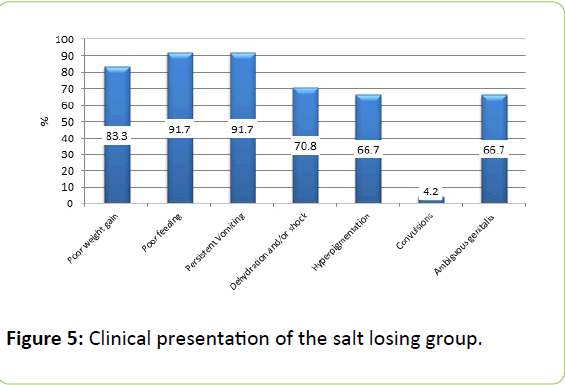
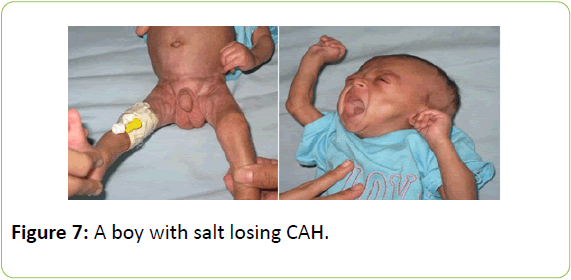
According to clinical presentation of salt losing group in our study 24 cases were in the salt losing group, 8 cases (33.3%) were males, 16 cases (66.7%) were females, the mean age at diagnosis in this group was 3 months, the salt losing group was presented with persistent vomiting in 22 cases (91.7%), poor feeding in 22 cases (91.7%), poor weight gain in 20 cases (83.3%), dehydration and/or shock in 17 cases (70.8%), hyperpigmentation in 16 cases (66.7%), ambiguous genitalia in 16 cases (66.7%) and convulsions in 1 case (4.2%). Our results are in agreement with [20,21] who reported that patients with severe salt wasting present at 2–3 weeks of life with adrenal crises, which includes vomiting, weight loss, lethargy, dehydration, hyponatraemia, hyperkalaemia and shock. This problem is particularly critical in male infants who have no genital ambiguity to alert physicians to the possibility of CAH [20]. Also, reported that female infants with classic CAH typically have genital ambiguity at birth because of exposure to high concentrations of androgens in utero. Characteristic findings include an enlarged clitoris, partly fused and rugated labia majora, and a common urogenital sinus in place of a separate urethra and vagina. The internal female organs, the uterus, fallopian tubes, and ovaries, are normal. Male infants however have no obvious signs of CAH at birth, except hyperpigmentation and possible subtle penile enlargement.
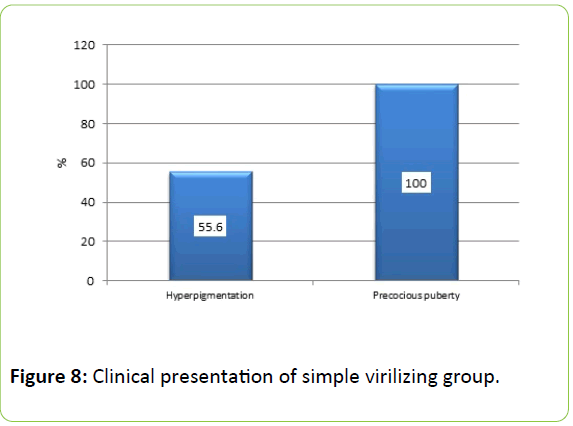
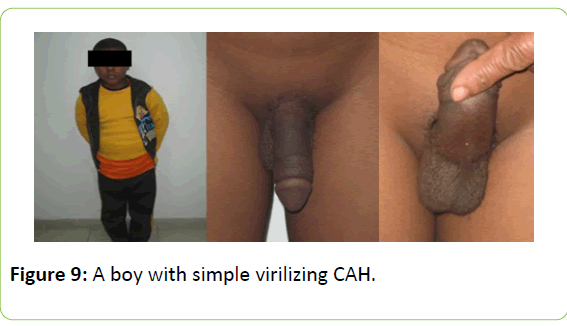
According to clinical presentation of simple virilizing group in our study, 9 cases were in the simple virilizing group, 6 cases (66.7%) were males, 3 cases (33.3%) were females, the mean age at diagnosis in this group was 4.2 years, and the simple virilizing group was presented with precocious puberty in 9 cases (100%) and hyperpigmentation in 5 cases (55.6%) (7). reported that classic simple virilizing type is characterized by progressive virilization, but no or mild evidence of mineralocorticoid deficiency [20,21] also reported that affected males may go undetected for several years, until symptoms and signs of androgen excess develop. The age at diagnosis in boys varies according to the severity of aldosterone deficiency [22]. also had reported through a five-year retrospective study on inpatients who had CAH as a final or presumptive diagnosis at the children’s hospital of Damascus between 2008–2012, or were diagnosed elsewhere and then admitted at the hospital for the first time within the same period that virilization was the most common manifestation among this group followed by vomiting.
Among the studied cases, 1 female case was in the non-classic group, diagnosed at the age of 9 years she was presented by premature pubarche, hirsutism, acne and hoarseness of voice [8] reported that non-classic type is a mild form that may be asymptomatic or associated with signs of postnatal androgen excess only.
According to laboratory presentation of salt losing group in our study, the salt losing group showed hypoglycemia in 20 cases (83.3%), hyponatremia and hyperkalemia in 21 cases (87.5%), metabolic acidosis in 18 cases (75%), increased renal chemistry in 5 cases (20.8%), increased serum 17(OH) progesterone in 24 cases (100%), decreased serum cortisol a.m and p.m in 20 cases (83.3%) and increased serum ACTH in 24 cases (100%).
According to laboratory presentation of simple virilizing group in our study, the simple virilizing group showed normal random blood sugar, serum electrolytes, kidney function tests, arterial blood gas, increased serum 17(OH) progesterone in 9 cases (100%), decreased serum cortisol a.m and p.m in 6 cases (66.7%), increased serum ACTH in 9 cases (100%) and increased serum testosterone in 9 cases (100%).
The non-classic group showed normal random blood sugar, serum electrolytes, kidney function tests, arterial blood gas, borderline serum17(OH) progesterone, but increased with ACTH stimulation test, decreased serum cortisol a.m and p.m increased serum testosterone and polycystic ovaries in pelviabdominal ultrasonography.
Patients with salt-losing disease have typical laboratory findings associated with cortisol and aldosterone deficiency, including hyponatremia, hyperkalemia, metabolic acidosis, and often, hypoglycemia, but these abnormalities can take 10-14 days or longer to develop after birth [1].
An elevated level of 17OHP is the biochemical hallmark of 21OHD and the main substrate for the 21-hydroxylase enzyme. Blood levels of 17-hydroxyprogesterone are markedly elevated. However, levels of this hormone are high during the 1st 2-3 days of life even in unaffected infants and especially if they are sick or premature leading to false positive results in newborn screening for congenital adrenal hyperplasia. Due to its circadian rhythm being concordant with cortisol [9], an early morning serum/ plasma 17OHP sample is used for screening. After infancy, once the circadian rhythm of cortisol is established, 17- hydroxyprogesterone levels vary in the same circadian pattern, being highest in the morning and lowest at night. Blood levels of cortisol are usually low in patients with the salt losing type of disease. They are often normal in patients with simple virilizing type of disease but inappropriately low in relation to the ACTH and 17-hydroxyprogesterone levels. Testosterone is elevated in affected females; testosterone is not elevated in affected males, because normal infant males have high testosterone levels compared with those seen later in childhood. ACTH levels are elevated but have no diagnostic utility over 17- hydroxyprogesterone levels [1].
Limitations
(1) Small sample size of our study due to short duration of the study (1 year).
(2) Financial constrains of investigations as assessment of other intermediate metabolites as deoxycorticosterone, dehydroepiandrosterone and dehydroepiandrosterone sulphate and genetic analysis.
(3) Neonatal screening of CAH is not done in Egypt.
Conclusion
CAH affects a considerable number of children in our locality. The majority of cases were diagnosed in the age range 1-12 months. The high incidence of CAH in our locality is due to increased rates of consanguineous marriage (33%) and even higher in Upper Egypt (up to 60%). Salt losing type of CAH is more common than simple virilizing type. Virilization is the most common presentation among the studied cases followed by persistent vomiting, dehydration and hyperpigmentation. High Serum 17-hydroxyprogesterone in a random blood sample is diagnostic of classic 21-hydroxylase deficiency.
Recommendations
(1) Any case with hyponatremia and hyperkalemia should be considered CAH until proved otherwise and should be well treated to avoid mortality.
(2) Any newborn with ambiguous genitalia should be fully investigated to exclude CAH.
(3) More effort is also required to educate the public regarding the disease presentation.
(4) The introduction of a neonatal screening program in Egypt is mandatory so that CAH can be diagnosed early leading to fewer patients presenting with life threatening adrenal crisis.
(5) Implementation of genetic analysis of cases of CAH is required to give better counselling of parents.
References
- White PC (2009) Neonatal screening for congenital adrenal hyperplasia, Nat Rev Endocrinol 5: 490–498.
- Turcu AF, Auchus RJ (2015) The next 150 years of congenital adrenal hyperplasia. Steroid Biochem Mol Biol 153: 63–71.
- Speiser PW, Azziz R, Baskin LS, Ghizzoni L, Hensle TW, et al. (2010) congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 9: 4133-4160.
- Witchel SF, Azziz R (2010) Nonclassic congenital adrenal hyperplasia, Int J Pediatr Endocrinol 625-105.
- Lee PA, Nordenström A, Houk CP, Ahmed SF, Auchus R, et al. (2016) Global disorders of sex development update since 2006: perceptions, approach and care. Horm Res Paediatr 3: 158-180.
- Ramadan MA, Itamid FA, Hofez MH (1999) Prevalence of late-onset congenital adrenal hyperplasia in 100 Egyptian women diagnosed as polycystic ovarian syndrome. Middle East Fertil Soc J 4-58.
- Speiser PW, White PC (2003) congenital adrenal hyperplasia. N Engl J Med 8: 776-788.
- Merke DP, Cutler GB (2001) new ideas for medical treatment of congenital adrenal hyperplasia. Endocrinol Metab Clin North Am 30: 121–135.
- Gutai Jp, Meyer Iii Wj, Kowarski Aa, Migeon Cj (1977) Twenty-four hour integrated concentrations of progesterone, 17-hydroxyprogesterone and cortisol in normal male subjects. J Clin Endocrinol Metab 1: 116-120.
- Maiti A, Chatterjee S (2011) Congenital adrenal hyperplasia: An Indian experience. J Paediatr Child Health 47: 883-887.
- Gidlöf S, Falhammar H, Thilén A, von Döbeln U, Ritzén M, et al. (2013) One hundred years of congenital adrenal hyperplasia in Sweden: a retrospective, population-based cohort study. Lancet Diabetes Endocrinol 1: 35–42.
- Thambiah S C, Ahmad Z, Hambal Z, Osman M, Zain MM et al. (2015) Clinical Presentation of Congenital Adrenal Hyperplasia in Selected Multiethnic Paediatric Population. Malaysian Journal of Medicine and Health Sciences 1: 77-83
- Wu LL, Krob G, Pekarak J, Hasrl BS, Kuhnle U (1994) 119 HIGH FREQUENCY OF CLASSICAL 21-HYDROXYLASE DEFICIENCY (CAH) IN MALAYSIA. Pediatr Res 1: 22A.
- THILÉN A, LARSSON A (1990) Congenital Adrenal Hyperplasia in Sweden 1969-1986 Prevalence, Symptoms and Age at Diagnosis. Acta Paediatr 79: 168–175.
- Virdi NK, Rayner PH, Rudd BT, Green A (1987) Should we screen for congenital adrenal hyperplasia? A review of 117 cases. Arch Dis Child 62: 659–662
- Kovács J, Votava F, Heinze G, Sólyom J, Lebl J, et al. (2001) Lessons From 30 Years of Clinical Diagnosis and Treatment of Congenital Adrenal Hyperplasia in Five Middle European Countries. J Clin Endocrinol Metab 86: 2958–2964.
- Lessons KJ (2001) from 30 Years of Clinical Diagnosis and Treatment of Congenital Adrenal Hyperplasia in Five Middle European Countries. J Clin Endocrinol Metab 86: 2958–2964.
- Menon PSN, Virmani A, Sethi AK, Verma IC, Rohatgi M, et al. (1992) Congenital adrenal hyperplasia: Experience at intersex clinic, AIIMS. Indian J Pediatr 59: 531–535.
- Bajpai A, Kabra M, Menon PS (2004) 21-Hydroxylase deficiency: clinical features, laboratory profile and pointers to diagnosis in Indian children. Indian Pediatr 41: 1226–1232.
- Merke DP, Bornstein SR (2005) congenital adrenal hyperplasia. The Lancet 365: 2125–2136.
- Khemiri M, Ridane H (2006) 11 beta hydroxylase deficiency: a clinical study of seven cases. Tunis Medical 84: 106-113.
- Alshabab LI, Alebrahem A, Kaddoura A, Al-Fahoum S (2015) congenital adrenal hyperplasia due to 21-hydroxylase deficiency: A five-year retrospective study in the Children's Hospital of Damascus, Syria. Qatar Med J 11.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences