Impacted Teeth and Early Detection of Hypoparathyroidism: A Rare Case Report with Literature Review
K. V. Chalapathi, Shazima Sheereen, S. Manoj Kumar, Zuber Ahamed Naqvi, Farheen Anjum Taqdeerullah Khan, Balagangadhar Tilak P and Abhishek Singh Nayyar*
1Department of Oral Pathology and Microbiology, Care Dental College and Hospital, Guntur, Andhra Pradesh, India
2Department of General Pathology, Kasturba Medical College, Manipal Academy of Higher Education, Mangalore, Karnataka, India
3Department of Oral Radiology, College of Dentistry, University of Ha’il, Ha’il, Kingdom of Saudi Arabia
4Department of Preventive Dental Sciences, Division of Orthodontics, College of Dentistry, Majmaah University, Majmaah, Kingdom of Saudi Arabia
5Department of Oral Medicine and Radiology, Swargiya Dadasaheb Kalmegh Smruti Dental College and Hospital, Nagpur, Maharashtra, India
6Department of Oral and Maxillofacial Surgery, Dr.Hedgewar Smruti Rugna Seva Mandal's Dental College and Hospital, Hingoli, Maharashtra, India
7Department of Oral Medicine and Radiology, Saraswati-Dhanwantari Dental College and Hospital and Post-Graduate Research Institute, Parbhani, Maharashtra, India
- *Corresponding Author:
- Nayyar AS
Department of Oral Medicine and Radiology
Faculty of Dentistry, Maharashtra University of Health Sciences
Nashik, Maharashtra, India
Tel: +91-98509 04067
E-mail: singhabhishekndls@gmail.com
Received date: October 05, 2018; Accepted date: November 08, 2018; Published date: November 15, 2018
Citation: Chalapathi KV, Sheereen S, Kumar SM, Naqvi ZA, Khan FAT, et al. (2018) Impacted Teeth and Early Detection of Hypoparathyroidism: A Rare Case Report with Literature Review. J Clin Mol Endocrinol 3: 3. doi: 10.21767/2572-5432.100048
Copyright: © 2018 Chalapathi KV. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Hypoparathyroidism is a rare endocrinological disorder accompanied by anomalies of various systems, bones and teeth. If diagnosed within first 10 years after birth and devoid of etiology, the condition is termed as idiopathic hypoparathyroidism (IHP). The dental defects due to hypoparathyroidism may present as hypocalcaemia, aplasia and/or, hypoplasia of enamel, incomplete mineralization of dentin, short and blunted roots, blunted molar apices, delayed eruptions and missing or, impacted teeth. Retention of multiple primary teeth and impacted permanent teeth can, also, be associated with various other syndromes or, hormonal and metabolic disorders. Early detection of this disorder is vital for effective management not only paving way for prevention of further dental damage progression, but, also, in improving the medical management and related outcomes. This case report elaborates a rare case where multiple impacted permanent teeth and retained primary teeth accompanied by other clinical manifestations led to further investigations which, eventually, helped in the early diagnosis of hypoparathyroidism.
Keywords
Impacted teeth; Hypoparathyroidism; Early detection; Idiopathic
Introduction
The endocrine system is responsible for the secretion of hormones which control the physiological processes and maintain homeostasis in the body. The endocrine system is closely related to the central nervous system as it diversifies its functions through the hypothalamus and pituitary [1]. One of the important endocrine glands in these are the parathyroid glands which consist of four small glands (3 mm × 6 mm × 2 mm) which are paired and located behind the thyroid gland in the neck. Parathyroid glands produce and release parathyroid hormone (PTH), which is involved in regulating the metabolism of calcium and phosphorus. Hyperparathyroidism (HPT) was first described by Von Recklinghausen in 1891. It results from excessive secretion of parathyroid hormone (PTH) with consequent osteoclastic resorptions and subsequent, hypercalcemia. It occurs in about 0.05%-0.1% of the population and is 2-3 times more prevalent in women than men with the male:female ratio for hypoparathyroidism being 1:3. Hypoparathyroidism is a relatively rare disorder which is identified by absence or, abnormally low levels of parathyroid hormone (PTH), low serum levels of calcium and elevated serum levels of phosphorus in blood circulation. It presents as a major therapeutic challenge which includes effectual management of the balance between treating hypocalcemia and simultaneously, avoiding hypercalciuria. The etiology of this disease is attributed to hereditary (autosomal dominant, recessive and X-linked), autoimmune, and the various acquired causes [1]. Hypoparathyroidism has known adverse effects on the development of tooth and its eruption which may manifest as the retention of primary teeth, impaired upper and lower jaw growth, alteration of facial dimensions and a shortfall of coordination in lower jaw growth which affects the development of dentition [2]. It may, also, present as brown tumors, eruption delays, impaction of teeth, and teeth with short and blunted roots [3,4]. The oral health care professional should, thus, be familiar with the oral and systemic manifestation of the parathyroid disease. Patients with a history of parathyroid disease should be carefully evaluated at the level of medical management and consultation with the patient's physician or, endocrinologist should be done. Furthermore, it is necessary to be aware of the common oral manifestations associated with these disorders and difficulties that may arise during the dental management of such patients. Eruption is a continuous process of movement of the developing tooth bud from its developmental location to functional location. Teeth that cease to erupt before emergence are termed as impactions. A tooth is termed as impacted if it fails to proceed from its developmental location inside the jawbone to its eventual functional location i.e., the occlusal plane. Various factors at genetic, cellular and molecular levels interplay in successful tooth eruption [5]. In permanent dentition, third molars are the most frequently impacted teeth followed by the canines. In decreasing order of frequency, impaction is seen with mandibular premolars, mandibular canines, maxillary premolars, maxillary central incisors, maxillary lateral incisors and mandibular second molars. First molars and maxillary second molars are rarely affected. When impaction involves few teeth, the condition is localized but when it involves multiple teeth, the condition becomes generalized. It is not a rarity to find impaction of a single tooth but a rarity to find multiple impacted teeth. Impaction can be owing to physical reasons like insufficient space, early closure of space, crowded arches or, thickened overlying bone or, soft tissues. The factors considered pathological causing impactions, likewise, may be local including overlying cysts or, tumors and trauma or, systemic conditions including hypoparathyroidism etc. Various syndromes, metabolic and hormonal disorders are, also, attributed to impactions [6-8]. As hypoparathyroidism presents early oral manifestations, an oral health care physician can play a major role in the early diagnosis and a central role in the multidisciplinary management of this disorder. This case report elaborates a rare case where multiple impacted permanent and retained primary teeth associated with other clinical findings, on further investigations, led to the diagnosis of hypoparathyroidism.
Case Report
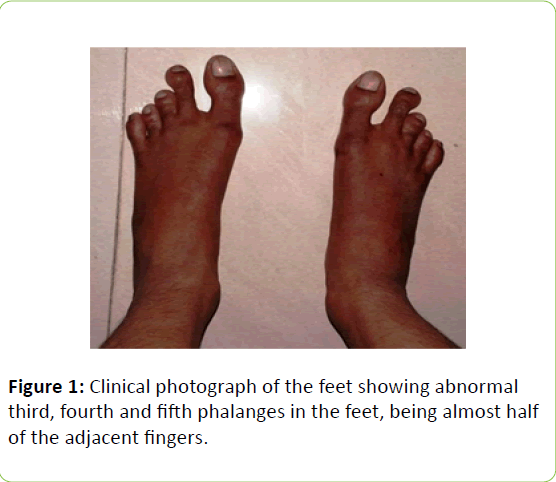
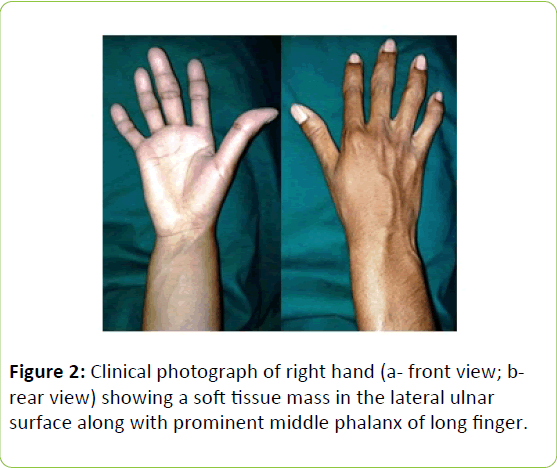
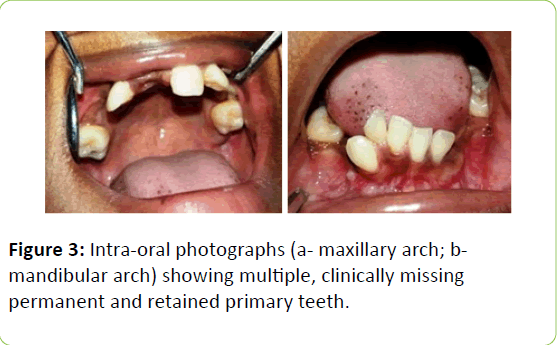
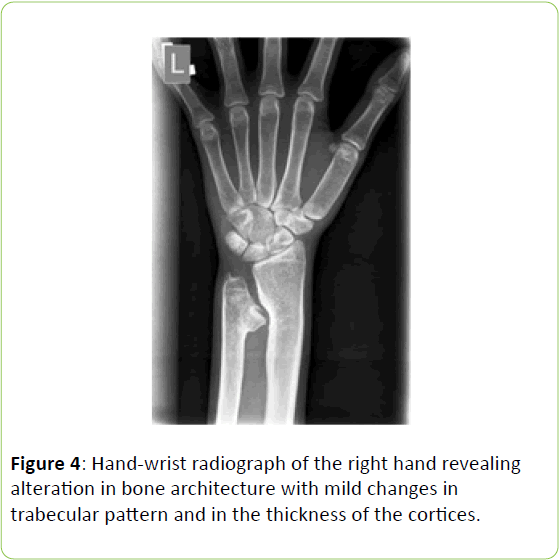
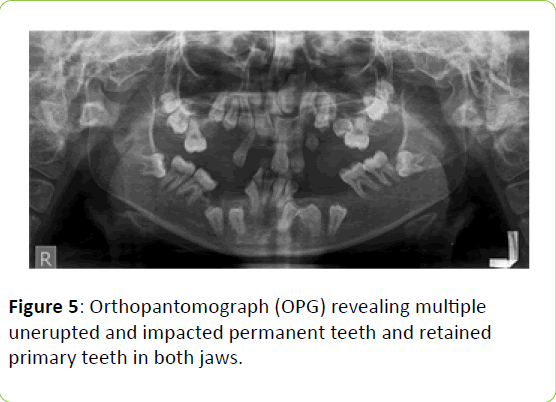
A 16-year-old female patient reported as an outpatient to the Department of Oral Medicine and Radiology with a chief complaint of multiple missing teeth. Her past dental history revealed usual loss of primary teeth with subsequent failure of eruption of the permanent teeth leading to difficulty in mastication. Her family history was positive for a consanguineous marriage of her parents. Her brother was negative for this issue. On general physical examination, the patient was conscious, cooperative, of moderate built and welloriented to time and place and the surroundings. Bilateral feet examination revealed an abnormal decrease in the size and diameter of the third, fourth and fifth phalanges when compared to the first two fingers of the feet (Figure 1). The lateral ulnar surface of the right hand showed a mass of soft tissue along with a prominent middle phalanx of the long finger (Figures 2a and 2b). No other abnormalities were observed w.r.t her physical or, mental abilities. Intra-oral examination revealed multiple retained deciduous teeth w.r.t # 63,65 with multiple missing permanent teeth w.r.t # 17,15,14,12,11,22,23,24,25,27,33,34,35,44 and 45 (Figure 3a and 3b). Based on the clinical examination, a provisional diagnosis was made as oligodontia of the maxilla and mandible. Differential diagnoses included hypothyroidism, hypoparathyroidism, cleidocranial dysplasia and Gardener's syndrome. A series of radiographic and serological examinations were planned. A hand-wrist radiograph of the right hand revealed alteration in the bone architecture with mild changes in the trabecular pattern and in the thickness of the cortices (Figure 4). Orthopantomograph (OPG) of the patient revealed multiple unerupted and impacted permanent teeth and retained primary teeth in both the jaws. The impacted teeth showed various levels of impactions in the anterior and posterior areas of the mandible, maxillary tuberosity, nasal floor and zygomatic region (teeth # 17,15,14,12,11,22,23,24,25,27,33,34,35,44 and 45). No evidence of cystic change was observed. The maxillary and mandibular bones displayed a mild ground glass appearance with faint trabecular pattern and an altered density. Mild blunting of mandibular molar roots was, also, evident (Figure 5). Serological investigations were done to evaluate serum calcium, phosphorous, serum alkaline phosphatase, PTH and thyroid hormone levels and vitamin D profile. The investigatory results revealed a decrease in calcium levels (8.15), increase in phosphorous (6.49) and TSH (6.79) and markedly decreased levels of PTH (<1.2). T3 and T4 levels were, though, found to be normal. Based on the clinical presentation, abnormal phalanges in the feet bilaterally, radiological and serological investigations, a final diagnosis of hypoparathyroidism was arrived-at. After counseling, the patient was advised to undergo thyroid function tests. The immediate target was to achieve normal test values. A multidisciplinary approach was adopted for treatment plan. After basic oral prophylaxis was performed, all the retained deciduous teeth were extracted. As most of the impacted teeth were vertically oriented, orthodontic procedure was drafted. The oral rehabilitation and visit to a physician are ongoing for effective management of hypoparathyroidism.
Discussion
Generally, tooth impaction is a common phenomenon [9]. However, impaction of multiple teeth is rare and is associated with metabolic disorders or, syndromes [10,11]. The reasons for impaction are linked to idiopathic, local or, systemic causes. The local factors can be regional odontodysplasia, mucosal barrier, radiation damage and the arch-length deficiency, to name a few. The common systemic causes include, although, not limited to, hypothyroidism, hypoparathyroidism, nutritional disturbances, vitamin D-resistant rickets, osteopetrosis, Gardner’s syndrome and cleidocranial dysplasia. Idiopathic causes can be due to abnormal eruptive forces, trauma to tooth germs and defects in the mechanism of the eruption [12,13]. According to Bayar et al., multiple impacted and unerupted teeth are frequently associated with Gardner’s syndrome or, cleidocranial dysplasia [14]. Hypoparathyroidism, a parathyroid hormone (PTH) deficiency abnormality, is secondary to various factors including genetic, surgical, autoimmune, radioactive iodine treatment and/or, certain systemic diseases and syndromes like DiGeorge, Schprintzen, and velo-cardio-facial syndrome [15-17]. A decreased level of PTH leads to calcium and phosphorus imbalance leading to hypocalcemia and hyperphosphatemia. Hypocalcemia may manifest as tetany, myalgia, dysphagia, irritability, anxiety, depression, psychosis and convulsions, all being the clinical signs and symptoms of a generalized increased neuromuscular excitability. Increased neuromuscular excitability (due to hypocalcemia) may, also, be demonstrated by eliciting Chvostek (twitching of the facial muscles in response to tapping over the facial nerve) or, Trousseau (carpopedal spasm induced by pressure applied to the arm by an inflated sphygmomanometer cuff) signs. In a positive Chvostek's sign, tapping the facial nerve at its point of origin (anterior to tragus of the ear) causes spasm of the facial musculature, particularly, of the lip and the alae of the nose while in a positive Trousseau sign, a carpopedal spasm is observed that results from ischemia such as that induced by pressure applied to the upper arm from an inflated sphygmomanometer cuff [18]. All these clinical features were, though, absent in the present case. The typical oral manifestations of this disorder include delayed eruption of permanent teeth, multiple retained primary teeth, horizontal lines of hypoplastic enamel, poorly calcified dentin, widened pulp chambers, dental pulp calcifications, short and blunted roots, blunt molar apices and hypodontia, evident, in the present case [2-4,19-24]. The primary and the permanent teeth were not subjected to ground sections to evaluate the exact level of defect in enamel and dentin. Two types of primary hypoparathyroidism have been described in the medical literature, namely, idiopathic hypoparathyroidism (IHP) and pseudo-hypoparathyroidism. The basic difference between the two lies in their response to treatment with parathormone and dihydrotachysterol (a form of vitamin D). In pseudohypoparathyroidism, the Ca levels return to normal following vitamin D treatment but not following parathormone (PTH) administration whereas IHP responds to both of these pharmacologic agents [25]. In both idiopathic and pseudohypoparathyroidism, fourth and fifth metatarsal as well as metacarpal bones appear quite short. Rarely, the third metatarsal or, metacarpal bone might, also, get affected. Hands and feet radiology studies, frequently, show quite significant and nearly diagnostic changes in the third, fourth and fifth metatarsal as well as metacarpal bones which can be almost half the magnitude of the adjacent, normal bones [26,27]. The dental manifestations of hypoparathyroidism are often ignored. The variations in formation as well as the eruption pattern of teeth can be critical in guiding additional investigations [28]. The present case revealed disturbances in the eruption pattern of the permanent teeth. The management of the disorder involves oral and intra-venous (i.v.) calcium, high doses of vitamin D as calcitriol and a diet rich in calcium and low phosphorus. The main treatments available for these patients are Vitamin D or, its analogs, calcium salts and drugs that increase renal tubular resorption of calcium to obtain adequate serum calcium levels [21]. Dental procedures can be started as per the need of the patient with proper medical management of the disorder and with periodic recalls. These patients have more susceptibility to caries because of dental anomalies for which periodic check-ups, advice regarding diet and oral hygiene instructions are highly recommended [2-4,19-24]. Enamel hypoplastic defects commonly seen in this set of patients, further, makes them more susceptible to develop carious lesions [24]. Also, pulp calcifications and malformed roots pose difficulty in endodontic treatment while ankylosis seen in these patients causes difficulty in extractions. Delayed eruption and hypodontia are other important considerations in patients affected with hypoparathyroidism that lead malocclusion in the early enough stages of the disease process and needs interceptive orthodontic treatment. The most important consideration in these patients is that before performing any kind of treatment, serum calcium levels should be assessed to prevent any susceptibility to develop complications in the form of cardiac arrhythmias, seizures and laryngospasms and/or bronchospasms which further leads to complications in and during carrying-out the treatment procedures [28].
Conclusion
Hypoparathyroidism shows early dental manifestations and it requires a careful assessment through clinical, radiographic as well as laboratory examinations. An oral health care physician must be vigilant to clinical oral manifestations like multiple impacted permanent and retained primary teeth and radiological observations including enamel hypoplasia, poorly calcified dentin, abnormally wide pulp chambers and short and blunted roots. Also, a short third, fourth, and fifth metatarsal and metacarpal bones can be suggestive of a hidden systemic disease. An early detection is a key to success in the effective management and oral health care physicians can play a vital role in it.
References
- Bilezikian JP, Khan AA, Potts JT Jr (2009) Guidelines for the management of asymptomatic primary hyperparathyroidism: Summary statement from the Third International Workshop. J Clin Endocrinol Metab 94: 335-339.
- Bedi R, Brook AH (1984) Changes in general, craniofacial and dental development in juvenile hypothyroidism. Br Dent J 157: 58-60.
- Kamarthi N, Venkatraman S, Patil PB (2013) Dental findings in the diagnosis of idiopathic hypoparathyroidism. Ann Saudi Med 33: 411-413.
- Walls AW, Soames JV (1993) Dental manifestations of autoimmune hypoparathyroidism. Oral Surg Oral Med Oral Pathol 75: 452-454.
- Wise GE, Frazier-Bowers S, D'Souza RN (2002) Cellular, molecular and genetic determinants of tooth eruption. Crit Rev Oral Biol Med 13: 323-334.
- Sujatha G, Sivapathasundharam B, Sivakumar G, Nalinkumar S, Ramasamy M, et al. (2012) Idiopathic multiple impacted unerupted teeth: Case report and discussion. J Oral Maxillofac Pathol 16: 125-127.
- Yildirim D, Yilmaz HH, Aydin U (2004) Multiple impacted permanent and deciduous teeth. Dentomaxillofac Radiol 33: 133-135.
- Kumar GS (2009) Orban's oral histology and embryology. 12th edition. India: Mosby.
- Chu FC, Li TK, Lui VK, Newsome PR, Chow RL, et al. (2003) Prevalence of impacted teeth and associated pathologies: A radiographic study of the Hong Kong Chinese population. Hong Kong Med J 9: 158-163.
- Gawande P, Hebbale M, Patil T, Hindocha A, Halli R (2015) Multiple impacted permanent and supernumerary teeth in the anterior mandible of non-syndromic case: A systematic review and multidisciplinary approach to management. J Dent Allied Sci 4: 47-51.
- Nayak UA, Mathian VM (2006) Non-syndrome associated multiple supernumerary teeth: A report of two cases. J Indian Soc Pedod Prev Dent 24: S11-S14.
- Sivakumar A, Valiathan A, Gandhi S, Mohandas AA (2007) Idiopathic failure of eruption of multiple permanent teeth: report of 2 adults with a highlight on molecular biology. Am J Orthod Dentofacial Orthop 132: 687-692.
- Nagaveni NB, Umashankara KV, Manjunath S (2011) Multiple impactions in non-syndromic patient: A case report. Arch Orofac Sci 6: 73-78.
- Bayar GR, Ortakoḡlu K, Sencimen M (2008) Multiple impacted teeth: Report of 3 cases. Eur J Dent 2: 73-78.
- Maeda SS, Fortes EM, Oliveira UM, Borba VC, Lazaretti-Castro M (2006) Hypoparathyroidism and pseudohypoparathyroidism. Arq Bras Endocrinol Metabol 50: 664-673.
- Garfield N, Karaplis AC (2001) Genetics and animal models of hypoparathyroidism. Trends Endocrinol Metab 12: 288-294.
- Graber ML (1995) Magnesium deficiency: Patho-physiologic and clinical overview. Am J Kidney Dis 25: 973.
- Nora DB, Fricke D, Becker J, Gomes I (2004) Hypocalcemic myopathy without tetany due to idiopathic hypoparathyroidism: Case report. Arq Neuropsiquiatr 62: 154-157.
- Frensilli JA, Stoner RE, Hinrichs EH (1971) Dental changes of idiopathic hypoparathyroidism: Report of three cases. J Oral Surg 29: 727-731.
- Jensen SB, Illum F, Dupont E (1981) Nature and frequency of dental changes in idiopathic hypoparathyroidism and pseudohypoparathyroidism. Scand J Dent Res 89: 26-37.
- Kelly A, Pomarico L, de Souza IP (2009) Cessation of dental development in a child with idiopathic hypoparathyroidism: A 5-year follow-up. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107: 673-677.
- Hansted C, Holst G (1952). Changes in dental tissue in hypoparathyroidism. Acta Odontol Scand 10:71-4.
- Takeuchi H, Hioki H, Ishikura Y, Tomizawa M, Noda T, et al. (1989) Dental findings in a case of idiopathic hypoparathyroidism. Shoni Shikagaku Zasshi 27: 678-691.
- Goepferd SJ, Flaitz CM (1981) Enamel hypoplasia associated with congenital hypoparathyroidism. Pediatr Dent 3: 196-200.
- Sprague RG, Haines E, Power RI (1945) Metabolic effects of parathyroid hormone, dihydrotachysterol and calciferol in case of pseudohypoparathyroidism. J Lab Clin Med 30: 363.
- Asa SL, Ezzat S (2005) Genetics and proteomics of pituitary tumors. Endocrines 28: 43-47.
- Mankin HJ, Jupiter J, Trahan CA (2011) Hand and foot abnormalities associated with genetic diseases. Hand (New York, NY) 6: 18-26.
- Laura Carlos Fabue l, Yolanda Jiménez Soriano, M Gracia Sarrión Pérez (2010) Dental management of patients with endocrine disorders. J Clin Exp Dent 2: e196-e203.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences